A new genetic therapy that helped blind mice and dogs respond to light stimulus could restore sight to people who suffer from diseases such as retinitis pigmentosa (a gradual loss of vision from periphery inwards). The therapy uses chemicals known as photoswitches, which change shape when hit with light, to open the channels that activate retinal cells. Treated mice can distinguish between steady and flashing light, while dogs with late-stage retinal degeneration also regain some sensitivity to light.
The procedure starts with an adeno-associated virus. Some retina cells in blind mice survive after disease kills the rod and cone photoreceptors, but they won't work on their own. The virus inserts a gene that instructs the cells to produce a modified version of a common glutamate receptor ion channel. Then photoswitches are attached to the newly-formed ion channels, akin to a glutamate amino acid dangling on a light-sensitive string. When light hits a photoswitch, it forces an ion channel open, thereby turning the retinal neurons on and off many times a second.
The researchers are able to insert the gene into almost all of the million or so retinal ganglion cells, which should restore useful vision. The success of this therapy will vary somewhat, however, depending on whether it targets early or late-stage retinal degeneration.
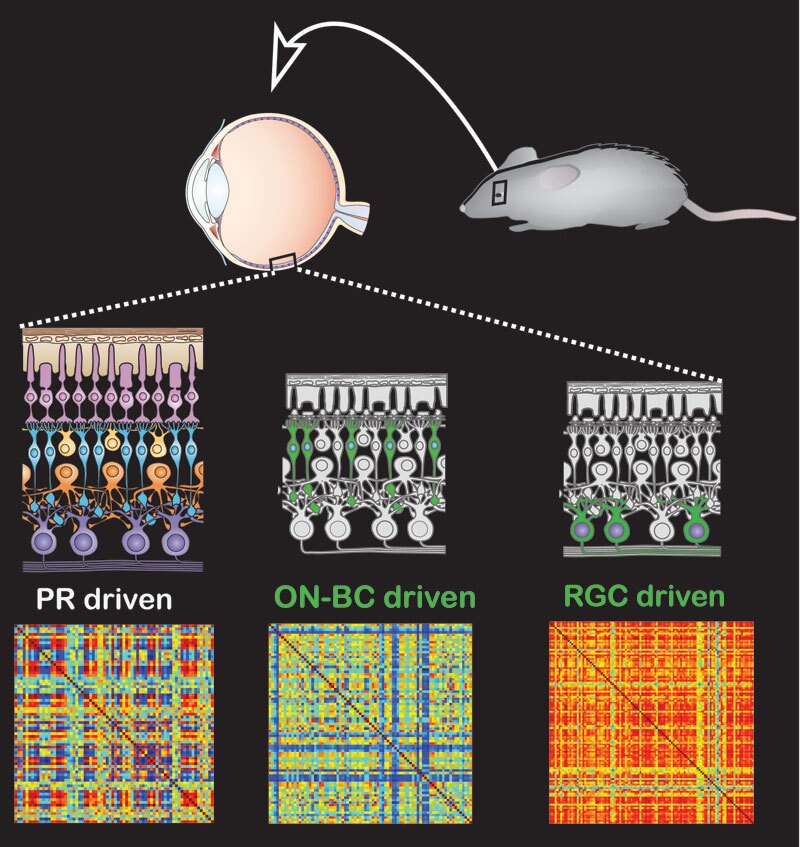
Mice in the early stages typically retain a functioning network of retinal cells – including both bipolar and ganglion types – but lack the photoreceptors to stimulate them, whereas mice in the later stages may have only the retinal ganglion cells. The later-stage group regained only basic, mostly-uniform responses to light – on or off signals – while the early-stage group's response to light was closer to that of normal mice. Both groups regained the ability to navigate a water maze at a comparable level to normal mice.
Blind dogs treated with the therapy also regained some vision. This is an encouraging sign for possible human applications.
"The dog has a retina very similar to ours, much more so than mice," explains lead researcher Ehud Isacoff, from the University of Berkeley, California. "So when you want to bring a visual therapy to the clinic, you want to first show that it works in a large animal model of the disease."
The dogs made a particularly good model for testing the therapy because they suffer from the same gene defect as that which often leads to retinitis pigmentosa in people. It's not clear yet what degree of light sensitivity they now have, but the researchers are nonetheless excited at the implications – which are boosted by the fact that the virus is already approved by the Food and Drug Administration for other genetic therapies in the eye.
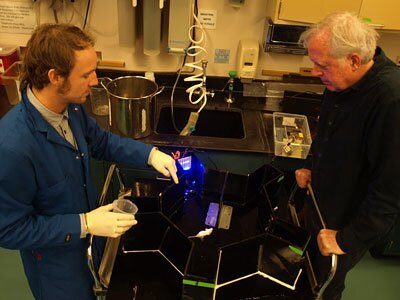
The next steps are to figure out how well the treated animals can distinguish between different images, to study how the dogs behave – especially those with photoswitches also inserted into bipolar cells – and to explore ways to improve the therapy. The animals currently need to be injected every week or so to resupply the chemical photoswitch, for instance, and there might also be ways to amplify the signal to allow perception of fainter light.
This is not the first case of gene or chemical therapy found to restore sight in mice suffering from retinitis pigmentosa. In 2010, a group of scientists in Paris developed a technique for repairing the function of cone photoreceptors via gene therapy, while a prior UC Berkeley study revealed a chemical compound that temporarily restores partial vision in a similar manner to this new research.
A paper describing the research was published in the journal Proceedings of the National Academy of the Sciences.
Source: UC Berkeley






