A few years ago I was rushed to hospital suffering anaphylaxis after eating a satay in peanut sauce. Although I'd previously experienced an itchy throat from eating nuts, I didn't realize at the time that this was an allergic reaction that could actually kill me. Luckily, friends got me to the hospital where I was shot full of adrenalin and everything was fine but, unfortunately, this is not always the result for many allergy sufferers. Now researchers have managed to rapidly turn off the allergic response to peanuts in mice by tricking the immune system into thinking the nut proteins aren't a threat.
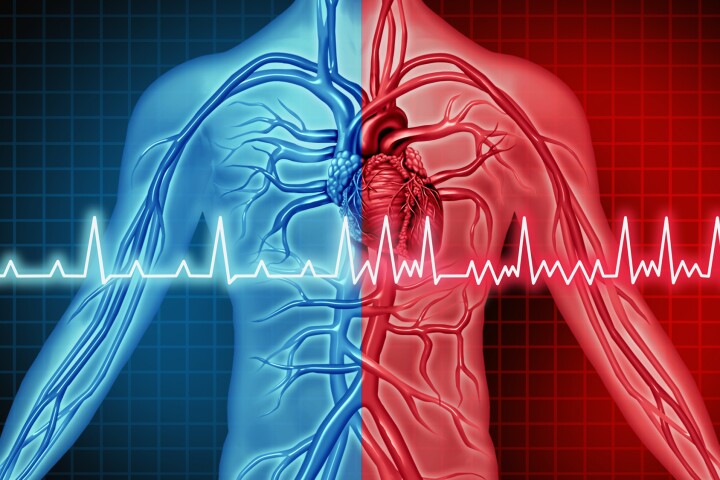
According to the National Institutes of Health, there are between 15,000 and 30,000 episodes of food-induced anaphylaxis and 100 to 200 related deaths in the U.S. alone every year. When an allergic person eats a peanut, the proteins are absorbed through the intestine and are mistakenly identified by the body's immune system as a threat. This can trigger a life-threatening, full-body immune response that includes constriction of the airways, low blood pressure and/or shock and can lead to loss of consciousness and death.
While some positive results have been seen in exposing peanut allergy sufferers to incrementally larger doses of peanuts to desensitize them to the allergy-causing protein, most people simply have to avoid the food in question. This is actually easier said than done. Even after I began religiously checking food labels and enquiring about exactly what was in a particular dish on a menu when eating out I still wasn't able to avoid accidentally eating peanuts on two occasions in the years since becoming aware of my allergy.
The approach by researchers at Northwestern University Feinberg School of Medicine could solve all these problems and actually let people with food allergies - not only to peanuts - enjoy the food they've so long been wary about. It involves attaching peanut proteins onto blood cells called leukocytes and reintroducing them into the body.
The researchers tested the approach using a mouse model that mimics a life-threatening peanut allergy. After two treatments, the mice were fed a peanut extract and didn't have an allergic reaction because their immune system now recognized the protein as safe.
"Their immune system saw the peanut protein as perfectly normal because it was already presented on the white blood cells," said Paul Bryce, PhD, an assistant professor of medicine in the division of allergy-immunology at Northwestern University Feinberg School of Medicine. "Without the treatment, these animals would have gone into anaphylactic shock."
Bryce believes that it should be possible to attach more than one protein to the surface of the blood cells to allow multiple food allergies to be targeted at the one time. Although the same approach has been used in treating autoimmune diseases, it is the first time this method for creating tolerance in the immune system has been used in allergic diseases. As an added benefit, the approach also increases the number of regulatory T cells, which are immune cells important for recognizing the peanut proteins as normal, resulting in a more normal, balanced immune system.
"T cells come in different 'flavors'," said Bryce. "This method turns off the dangerous Th2 T cell that causes the allergy and expands the good, calming regulatory T cells. We are supposed to be able to eat peanuts. We've restored this tolerance to the immune system."
In the second part of their study, the researchers tested the same approach with another common food allergy - egg protein - which provokes an immune response similar to an asthma attack in the lungs. Again, after the proteins were attached to white blood cells and infused back into the mice, they had no adverse effects after inhaling the asthma-provoking egg protein.
"This is an exciting new way in which we can regulate specific allergic diseases and may eventually be used in a clinical setting for patients," said Miller, the Judy Gugenheim Research Professor at Feinberg.
The Northwestern University team's research appears in a paper published in the Journal of Immunology.